It started as a simple rash. The kind you’d dismiss with a quick trip to the pharmacy for some antihistamines. But what doctors initially brushed off as a “common allergy” was actually a life-threatening condition that kills 30% of those it strikes.
This isn’t just one isolated case—it’s a terrifying pattern that’s happening in hospitals across the country. Medical professionals, pressed for time and overwhelmed by patient loads, are making snap judgments that could be fatal. And the scariest part? The patients who survive are often the ones who refused to accept the first diagnosis.
When Your Body Declares War on Itself
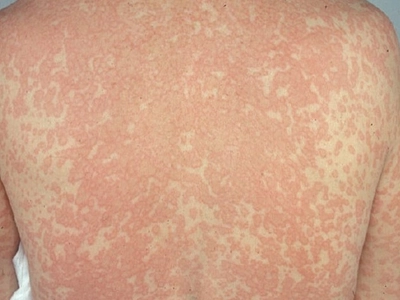
Toxic Epidermal Necrolysis (TEN) and Stevens-Johnson Syndrome (SJS) are medical emergencies that medical professionals frequently mistake for simple allergic reactions. These conditions cause your skin to literally die and peel off your body in sheets—like a severe burn victim, but from the inside out.
The initial symptoms are deceptively innocent: a rash, some itching, maybe a low-grade fever. Doctors see these signs and think “drug allergy” or “contact dermatitis.” They prescribe antihistamines and send patients home. But within hours or days, the patient’s condition explodes into a medical nightmare.
“I watched my husband’s skin fall off in my hands,” recalls Sarah Martinez, whose spouse was initially told he had a “mild drug reaction.” “The emergency room doctor said it was just an allergy and to take Benadryl. By the next morning, he looked like he’d been burned alive.”

The 15% Misdiagnosis Rate That’s Killing Patients
Recent studies reveal that 10-15% of all medical diagnoses are wrong—but when it comes to skin conditions, the numbers are even more alarming. DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms) is another killer that mimics common allergies. It affects multiple organ systems and can cause liver failure, kidney damage, and heart problems.
The tragic irony? These conditions are often triggered by the very medications doctors prescribe to treat the “allergy” they think they’re seeing.
Dr. James Chen, an emergency medicine physician who’s seen too many of these cases, admits: “We’re trained to look for horses, not zebras. But sometimes that zebra will kill you if you don’t catch it in time.”
The Patients Who Saved Their Own Lives
The survivors have one thing in common: they didn’t accept the first diagnosis.
Mark Thompson was told his spreading rash was “just eczema” and given steroid cream. But something felt wrong. “My wife said I was being paranoid, but I knew this wasn’t normal. I went to three different doctors before someone finally recognized what was happening.”
By the time Thompson got the correct diagnosis of SJS, his condition had progressed to the point where 25% of his skin was affected. He spent six weeks in a burn unit, but he’s alive because he trusted his instincts.
The Red Flags Doctors Are Missing
Certain warning signs should immediately trigger alarm bells, but they’re often overlooked:
- Rash that spreads rapidly within hours
- Blisters or skin that feels “loose” or slides off
- Fever accompanying a skin reaction
- Mouth sores or eye irritation with a rash
- Feeling systemically ill (beyond just the skin symptoms)
These aren’t just “allergy symptoms.” They’re your body’s distress signals screaming for immediate, intensive medical care.
Why Medical Training Is Failing Patients
Medical schools teach doctors to diagnose the most common conditions first—it’s called “clinical reasoning.” But this approach fails catastrophically when rare, life-threatening conditions present with common symptoms.
The pressure on emergency departments makes it worse. Doctors have minutes, not hours, to make decisions. Insurance companies push for quick turnarounds. The system is designed for speed, not accuracy.
“I’ve seen residents dismiss patients with serious conditions because they’ve been trained to think ‘common things are common,’” says Dr. Maria Rodriguez, who leads a diagnostic error prevention program. “But when you’re wrong about these skin conditions, people die.”
The Fight for Your Life Starts with Your Voice
The most important thing you can do is trust your instincts. If something feels wrong, keep pushing. Ask specific questions:
- “What else could this be besides an allergy?”
- “What are the warning signs I should watch for?”
- “If this gets worse, how quickly should I seek help?”
Don’t be afraid to seek a second opinion. Don’t let anyone make you feel like you’re being “difficult” or “anxious.” Your life might depend on your refusal to accept an inadequate diagnosis.
The Tragic Truth About Medical Hubris
The medical community has a dirty secret: diagnostic errors are the third leading cause of death in hospitals. But skin conditions are particularly vulnerable to misdiagnosis because they’re visible, and doctors think they can assess them quickly.
This false confidence kills.
The patients who survive aren’t necessarily the ones who get the best initial care—they’re the ones who refuse to be dismissed. They’re the ones who show up at the emergency room again when things get worse. They’re the ones who demand answers when their “allergy” doesn’t respond to treatment.
Your Life Is Worth More Than a Doctor’s Convenience
The next time you’re dealing with a mysterious rash or skin condition, remember: you know your body better than anyone else. If something feels wrong, it probably is. Don’t let medical professionals rush you out the door with a quick diagnosis and a prescription.
Your intuition isn’t just valuable—it might be the difference between life and death. Trust it.



